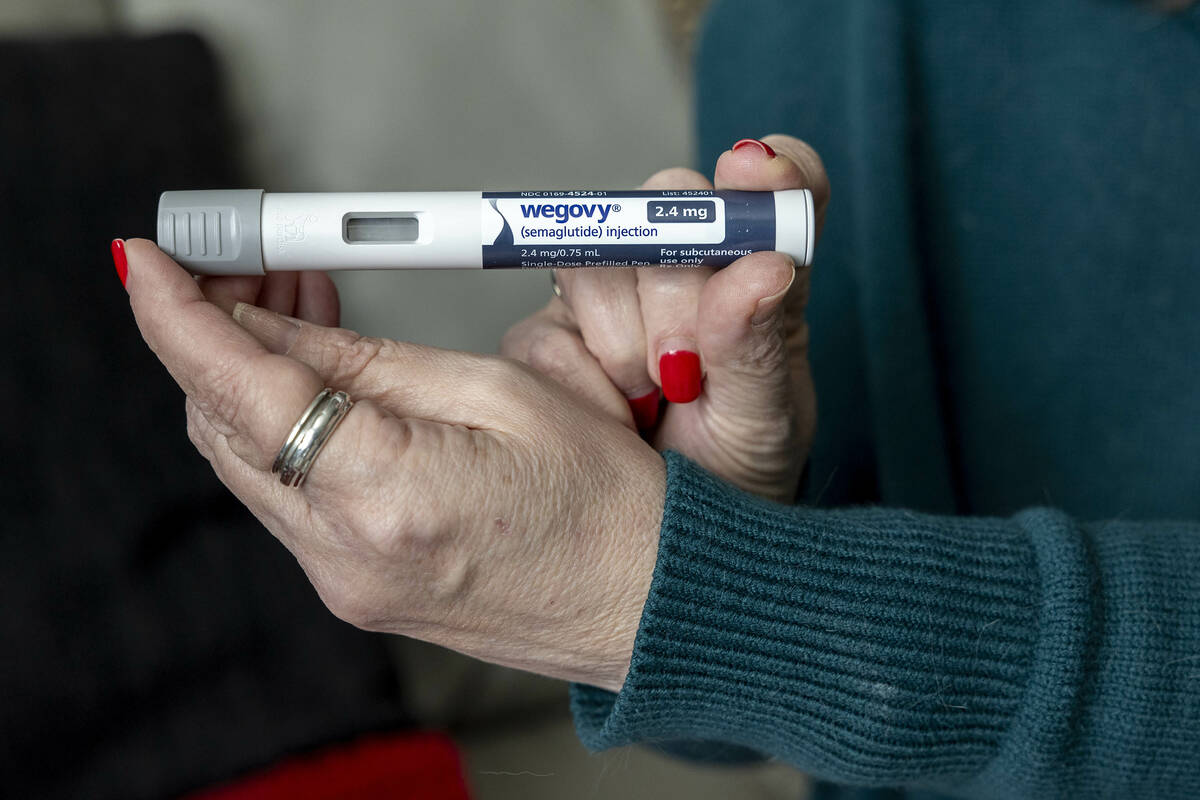
President Donald Trump has announced agreements with drug manufacturers Eli Lilly and Novo Nordisk aimed at reducing prices for GLP-1 weight-loss medications under Medicare and Medicaid. This move is part of a broader initiative to create a yet-to-be-developed online marketplace for prescription drugs, named TrumpRx. The agreements also involve price reductions for sales made through this platform.
Both Eli Lilly and Novo Nordisk join Pfizer and AstraZeneca in negotiating with the Trump administration to lower prices on selected medications. Trump has positioned these deals as a victory for his “Most Favored Nation” executive order, which intends to ensure that American consumers receive the best prices available in other developed countries. Notably, these agreements were made voluntarily, raising questions about the potential implications of implementing such pricing mandates into law.
Market Access and Strategic Benefits
The agreements offer significant advantages for the participating drug companies, particularly in accessing a previously restricted market. Historically, Medicare has not covered drugs prescribed for weight loss. This deal marks a shift, allowing beneficiaries with obesity to receive coverage for these medications. By reducing prices, the drugmakers stand to gain considerable market access.
While the agreements present a new approach, it is important to note that prior to these changes, drug companies were already required to sell medications to Medicaid at approximately 23 cents on the dollar. As a result, the difference between the newly announced deals and existing arrangements may not be as substantial as initially portrayed.
Trump’s administration aims to address the disparity in drug prices between the United States and other countries. Acknowledging that many Americans feel disadvantaged, the administration’s approach raises concerns regarding the impact of foreign price controls on pharmaceutical innovation. Countries like the United Kingdom and Australia often impose stringent pricing measures that can lead to reduced access to new treatments.
Implications for Innovation and Access
The potential adoption of foreign pricing models carries serious risks. In the UK, for instance, the public health system covers only 43 percent of innovative medicines, while in Australia, this figure drops to just 25 percent. These healthcare systems often evaluate the cost-effectiveness of new drugs using a metric known as the quality-adjusted life year (QALY), which assigns a value to an additional year of life without disability. In Britain, this value ranges between $27,000 and $40,000, while in the United States, it can be valued at four times that amount or more.
If the United States were to implement most-favored-nation pricing, it could hinder the availability of new drugs domestically. Research indicates that over half of all new drugs are first launched in the U.S., allowing American patients access to treatments up to a year earlier than those in Europe, Japan, or Australia. Implementing foreign pricing schemes could lead to delays in drug launches within the United States, ultimately affecting patient care.
A study published in September 2023 by economists from the University of Chicago highlights the potential consequences of adopting these pricing measures. The analysis suggests that applying most-favored-nation pricing to Medicare and Medicaid could reduce research and development spending by 48 percent, resulting in the loss of approximately 500 new treatments over a decade. This could contribute to the loss of around 6.6 million lives, underscoring the critical link between drug pricing policies and medical innovation.
As the debate surrounding drug pricing continues, American patients remain at the center of the discussion. The United States has long been seen as a leader in pharmaceutical innovation, and ensuring that this status is maintained is vital for future advancements in healthcare. The current agreements with Eli Lilly and Novo Nordisk represent a step towards addressing drug costs, but the broader implications of these policies must be carefully considered to safeguard access to life-saving medications for all.