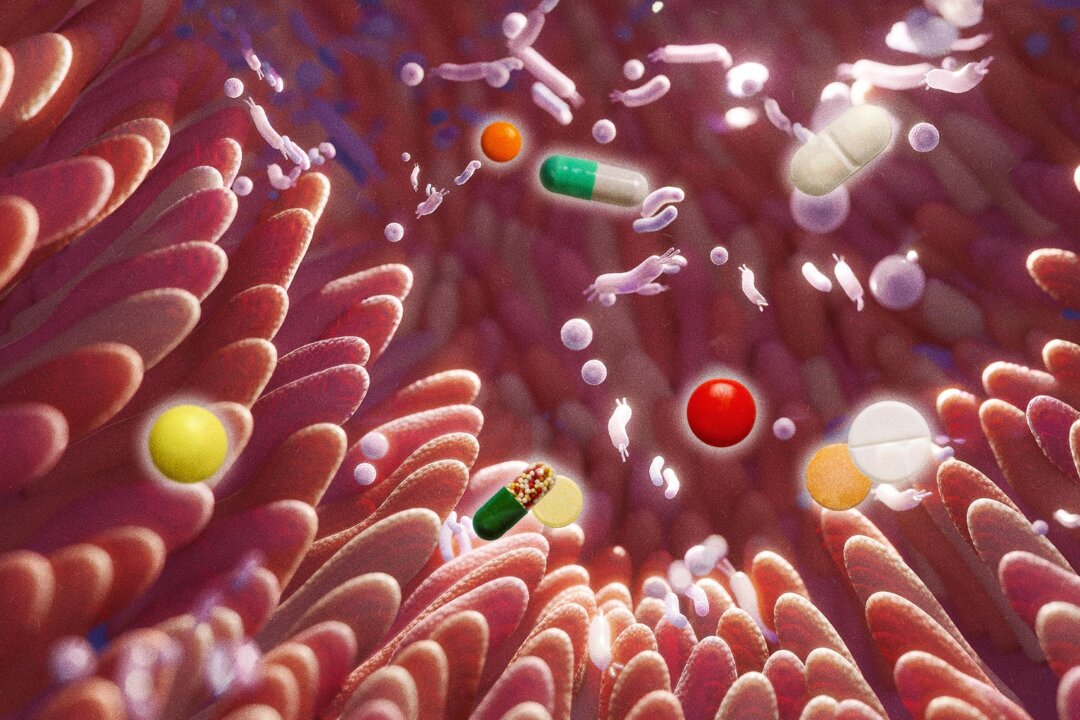
Research has revealed that approximately 28 percent of nonantibiotic medications can disrupt gut health, raising concerns over their impact on patients. This finding highlights a potential risk for the elderly and frail individuals who may already be vulnerable to infections. The study, led by Lisa Maier and published in the journal Nature, indicates that common medications—including allergy pills, antidepressants, and hormone treatments—can promote the growth of harmful pathogens.
The scale of the issue came as a surprise to researchers. In a laboratory setting, 53 tested nonantibiotic drugs were evaluated, with nearly a third found to encourage the growth of dangerous bacteria such as Salmonella. “The scale of it was utterly unexpected,” Maier stated in a press release. She emphasized that many of these nonantibiotic drugs inhibit beneficial gut bacteria while allowing pathogenic microbes to thrive.
Understanding the Implications
The gut microbiome plays a crucial role in maintaining overall health, acting as a barrier against harmful pathogens. The disruption of this balance can lead to serious intestinal infections, particularly in vulnerable populations. “This gives rise to an imbalance in the microbiome, which gives an advantage to the pathogens,” Maier explained.
This research underscores the need for healthcare providers to reconsider the potential side effects of nonantibiotic medications. Patients often take these medications without being aware of their possible implications on gut health. As the findings suggest, the risk is significant, especially for those with compromised immune systems.
Broader Context and Future Research
The implications of this study extend beyond individual patient care. With millions relying on these medications, understanding their effects on gut health is crucial. The research team calls for further studies to explore the long-term consequences of nonantibiotic drug use on the microbiome.
As the healthcare community grapples with these findings, it is essential for patients and providers alike to engage in informed discussions about medication choices. This study serves as a reminder of the complex interplay between medications and gut health, emphasizing the need for vigilance in prescribing practices.
In conclusion, the revelation that nonantibiotic drugs can disrupt gut health poses a significant challenge. Continued research and awareness are vital to safeguard the health of patients, particularly those at higher risk. The findings of this study could lead to more cautious prescribing habits and greater emphasis on the importance of gut microbiome health in medical treatments.