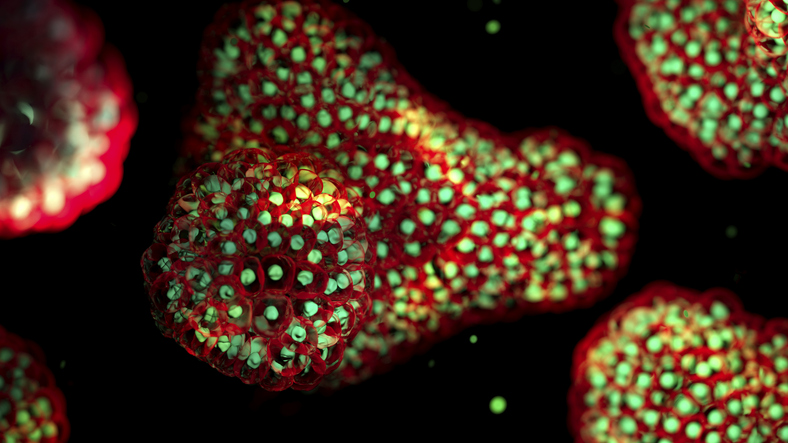
Understanding the complexities of human biology in response to environmental factors, known as “exposomes,” has taken a significant step forward with the advancement of human organoid technology. Researchers have begun using these three-dimensional (3D) structures to mimic human organs, allowing for a more accurate study of how these factors affect health. This innovative approach is critical, as traditional models often fall short in replicating human physiology.
Exposomes encompass a range of non-genetic influences that impact our health, such as pollutants, UV radiation, and other environmental stimuli. These factors are particularly relevant for the immune system, which can enter inflammatory states due to various exposures. Conventional research models, including two-dimensional (2D) cell cultures and animal testing, often fail to provide reliable data due to their inherent limitations. For instance, 2D cultures lack the necessary structural context, while animal models do not perfectly replicate human cellular makeup.
The recent announcement by the U.S. Food and Drug Administration (FDA) to reduce reliance on animal testing for therapeutic evaluations has accelerated the demand for more accurate organoid systems. This shift is motivating researchers to develop organoids that better reflect human biology and immune responses.
Breakthroughs in Immune Organoid Development
Despite organoids being in development for over two decades, the first immune organoids were only recently reported in 2021, with further advancements made in 2024. The work of Lisa Wagar, PhD, and her team at Stanford University demonstrated that immune organoids derived from tonsil tissues could retain 16 different immune cell types, including B and T cells, which are typically challenging to obtain from induced pluripotent stem cells (iPSCs). This retention of immune memory allows for more relevant personalized medicine applications.
Additionally, the immune organoids exhibited the ability to produce flu-specific antibodies when immunized, showcasing their capacity to simulate real immune responses. However, challenges remain, particularly regarding the tissue microenvironment, which can complicate further analyses.
In late 2024, researchers at the Georgia Institute of Technology reported a second immune organoid model that incorporated hydrogel biomaterials to better replicate the tonsil tissue environment. Their model produced clearer germinal centers but faced issues with hydrogel degradation, which compromised long-term viability. Nevertheless, they noted that their organoids could generate only a weak immune response against influenza.
AI Innovations in Organoid Research
The integration of artificial intelligence (AI) into organoid research is providing new methodologies for studying diseases. For instance, a team led by Haotian Bai, PhD, and Shu Wang, PhD, at the Chinese Academy of Sciences, developed a database to analyze the impact of inflammatory cytokines on heart organoids. Their AI model enabled rapid assessment of inflammation severity by analyzing various cytokine concentrations and exposure times. This approach revealed that treatment with interleukin-1β resulted in significant heart inflammation, providing insights into the mechanisms of cardiac dysfunction.
The researchers highlighted that their platform uniquely combines video-based radiomics with machine learning, allowing for rapid, quantitative assessments of organoid health. This innovation promises to streamline the evaluation process, making it faster and more scalable than traditional methods.
Another notable development comes from the field of oncology. Research by Nathalia Ferreira and her colleagues focuses on pancreatic ductal adenocarcinoma (PDAC), a notably aggressive cancer type. They developed patient-derived PDAC organoids and employed an AI algorithm named OrganoIDNet to monitor organoid response to therapeutic interventions. Their work aims to enhance the efficacy of personalized immunotherapy approaches, particularly for patients with challenging tumor environments.
Organoids are proving to be invaluable tools for mimicking human physiology and understanding how various exposomes impact health. The ongoing advancements in organoid technology, coupled with AI enhancements, are expected to accelerate biomedical research and therapeutic development.
As researchers continue to refine these systems and overcome existing challenges, the potential for organoids to revolutionize our understanding of human biology and disease response becomes increasingly apparent. The future of organoid research promises not only to deepen our understanding of exposomes but also to pave the way for more effective treatments tailored to individual patient needs.