Advancements in gene editing technology have gained significant momentum with researchers at the University of California Berkeley’s Innovative Genomics Institute unveiling a promising solution to enhance the nuclear entry of CRISPR-Cas9. This novel approach aims to improve the efficiency of gene editing in human T cells, a critical component in various cell therapies, including cancer treatments.
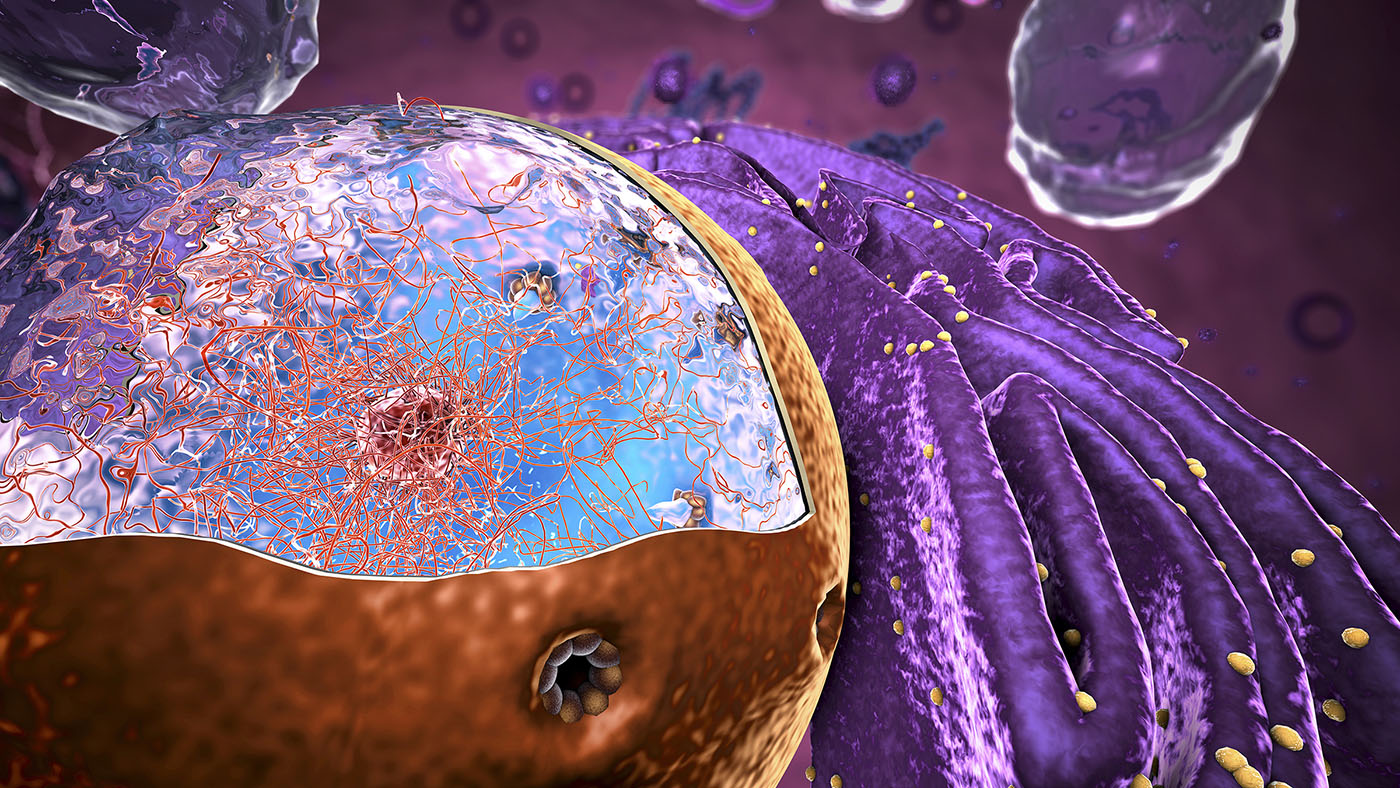
Current applications of CRISPR-Cas9 face limitations primarily due to challenges in delivering sufficient amounts of the Cas9 protein into the cell nucleus, where it performs essential modifications to DNA. Traditional methods have relied on adding nuclear localization signal (NLS) motifs, which facilitate nuclear entry. Unfortunately, these strategies often result in poor delivery efficiency, with a significant portion of Cas9 failing to reach its target.
Innovative Solution to Nuclear Entry
The Berkeley research team proposed that increasing the number of NLS motifs within the Cas9 protein could enhance its nuclear import. However, initial attempts to extend the protein’s terminal ends with additional NLS motifs resulted in low expression yields, complicating large-scale production. Instead, the researchers strategically inserted NLS motifs into internal loops of the Cas9 protein, achieving a more effective distribution across its structure.
This approach led to the development of hairpin internal NLS (hiNLS) modules, which consist of two NLS motifs arranged in tandem. This design ensures that if one motif detaches during the nuclear entry process, the other can maintain its connection, thereby increasing the likelihood of successful transport into the nucleus. The team successfully created 15 variants of Cas9 with up to nine individual NLS motifs.
Testing and Implications for T Cell Editing
To assess the efficacy of their hiNLS-Cas9 variants, the researchers conducted tests using primary human T cells. These cells are vital in therapies such as chimeric antigen receptor (CAR) T cells. The team introduced gRNA-Cas9 ribonucleoprotein complexes targeting two crucial genes: b2M (beta-2 microglobulin) and TRAC (T-cell receptor alpha chain). Disruption of the b2M gene can create immune-evasive cell therapies by eliminating the expression of major histocompatibility complex I (MHC-I) molecules on T cells. In contrast, targeting TRAC can help prevent graft-versus-host reactions.
The researchers employed two methods for delivering RNPs to cells: standard electroporation and a gentler peptide-mediated method known as PERC. Compared to electroporation, which can impact cell viability, PERC offers a simpler and less damaging alternative.
The results were promising. The Cas9 variant with two NLS modules (s-M1M4) delivered via electroporation knocked out the b2M gene in over 80% of T cells, a significant improvement compared to the 66% achieved with conventional Cas9. Additionally, several multi-hiNLS constructs reached knockout efficiencies of 40% to 50%, while the control showed around 38%. Throughout these experiments, T-cell viability remained unaffected by the added NLS motifs, indicating the potential for therapeutic applications.
While the study did not find a direct correlation between the number of NLS inserts and editing efficiency, it did reveal that variants enriched with c-Myc-derived NLS outperformed those featuring SV40 NLS signals. This suggests that the quality of the NLS sequence is equally important as the quantity.
The findings underscore the practical advantages of hiNLS-Cas9 for therapeutic development. By addressing the nuclear entry bottleneck, this enhanced version of Cas9 can achieve higher editing percentages in T cells than traditional methods. This improvement could benefit other difficult-to-edit cell types, making both experimental and therapeutic applications more effective.
Moreover, the hiNLS-Cas9 variants exhibited maintained protein yields, producing 4-9 mg per liter, comparable to unmodified Cas9. This efficiency means that laboratories can manufacture hiNLS-Cas9 at scale without requiring complex techniques, crucial for clinical translation.
Looking to the future, the researchers noted the potential for combining the hiNLS-Cas9 method with other advances in gene editing technology. Approaches such as virus-like particles and lipid nanoparticles could facilitate direct delivery of Cas9 RNPs in vivo. Enhanced nuclear localization may significantly improve outcomes in these applications, which often struggle with low delivery rates.
Additionally, researchers may explore engineering Cas9 for increased specificity. Early observations indicated a slight uptick in off-target activity with hiNLS-Cas9, likely due to the extended binding time on DNA afforded by the extra NLS motifs. Merging high-fidelity Cas9 mutations with hiNLS could yield an enzyme that is both accurate and highly efficient.
Ultimately, the hiNLS-Cas9 strategy reflects a critical shift in gene editing design, emphasizing the importance of nuclear localization in enhancing therapeutic efficacy. As the field moves toward multiplexed approaches, where multiple genes are targeted simultaneously, the efficiency of each individual edit becomes increasingly vital. The advancements discussed in this study could help accelerate the development of gene-edited cell therapies, potentially reducing manufacturing costs and benefiting patients awaiting these innovative treatments.
Christopher Doyle, PhD, serves as the senior director of IBC Services at WCG Clinical.