Prostate cancer stands as the most prevalent cancer among men, following skin cancer, with approximately 1 in 8 men receiving a diagnosis during their lifetime. This disease targets the prostate, a small gland located below the bladder that contributes to semen production. Understanding the risk factors, symptoms, and treatment options is crucial for early detection and effective management.
Understanding Prostate Cancer Risk Factors
Age significantly influences the likelihood of developing prostate cancer. According to the American Cancer Society, around 60% of prostate cancer cases occur in men aged 65 and older, with an average diagnosis age of 66. While prostate cancer is rare in men under 40, the risk escalates after age 50, reaching nearly 60% by age 80.
Family history also plays a critical role in risk assessment. Men who have a father, brother, or son diagnosed with prostate cancer face a 2 to 3 times higher risk. Medical professionals often recommend earlier screening, starting at ages 40–45, for those with a family history of the disease. Additionally, race and ethnicity contribute to risk disparities; African American men are 1.7 times more likely to be diagnosed and 2.1 times more likely to die from prostate cancer compared to non-Hispanic white men.
Recognizing Symptoms and Diagnostic Procedures
Early-stage prostate cancer typically presents with no symptoms. However, as the disease progresses, symptoms may arise, including difficulties with urination and the presence of blood in urine or semen. Any concerning symptoms should prompt consultation with a healthcare provider.
Most prostate cancers are initially detected through a Prostate-specific antigen (PSA) blood test. PSA, a protein produced by prostate cells, varies in concentration in the blood. While higher levels may indicate cancer, they do not definitively confirm its presence. If results suggest the possibility of prostate cancer, further diagnostic tests, including a prostate biopsy, are necessary. This procedure involves extracting tissue from the prostate for laboratory analysis.
Pathologists assess the biopsy samples using the Gleason Score, a grading system developed by Dr. Donald Gleason in the 1960s. This score reflects the aggressiveness of cancer based on the appearance of cancerous cells. Scores range from 6 to 10, with lower scores indicating less aggressive disease. Notably, the presence of any cells rated at Gleason grade 5 increases the risk of recurrence.
The staging of prostate cancer plays a pivotal role in treatment decisions. Stage 1 indicates localized cancer with a Gleason score of 6 or lower and a PSA level of 9 or lower. Stage 2 remains confined to the prostate, but the Gleason score rises to 7 or higher, and the PSA level is between 10 and 20. Stage 3 may still be confined to the prostate but presents a PSA level of 20 or higher, or the cancer has breached the outer layer of the prostate. Stage 4 signifies advanced disease that has spread to nearby lymph nodes, tissues, or distant organs.
The treatment landscape for prostate cancer is diverse, encompassing surgery, radiation therapy, hormone therapy, chemotherapy, targeted therapy, and immunotherapy. The choice of treatment depends on cancer size, metastasis, growth rate, and the patient’s overall health.
Despite the challenges posed by prostate cancer, the prognosis remains favorable. The five-year survival rate for localized cancer is nearly 100%, while it drops to 32% for advanced stages. With effective treatment options available, many men continue to lead long and healthy lives post-diagnosis.
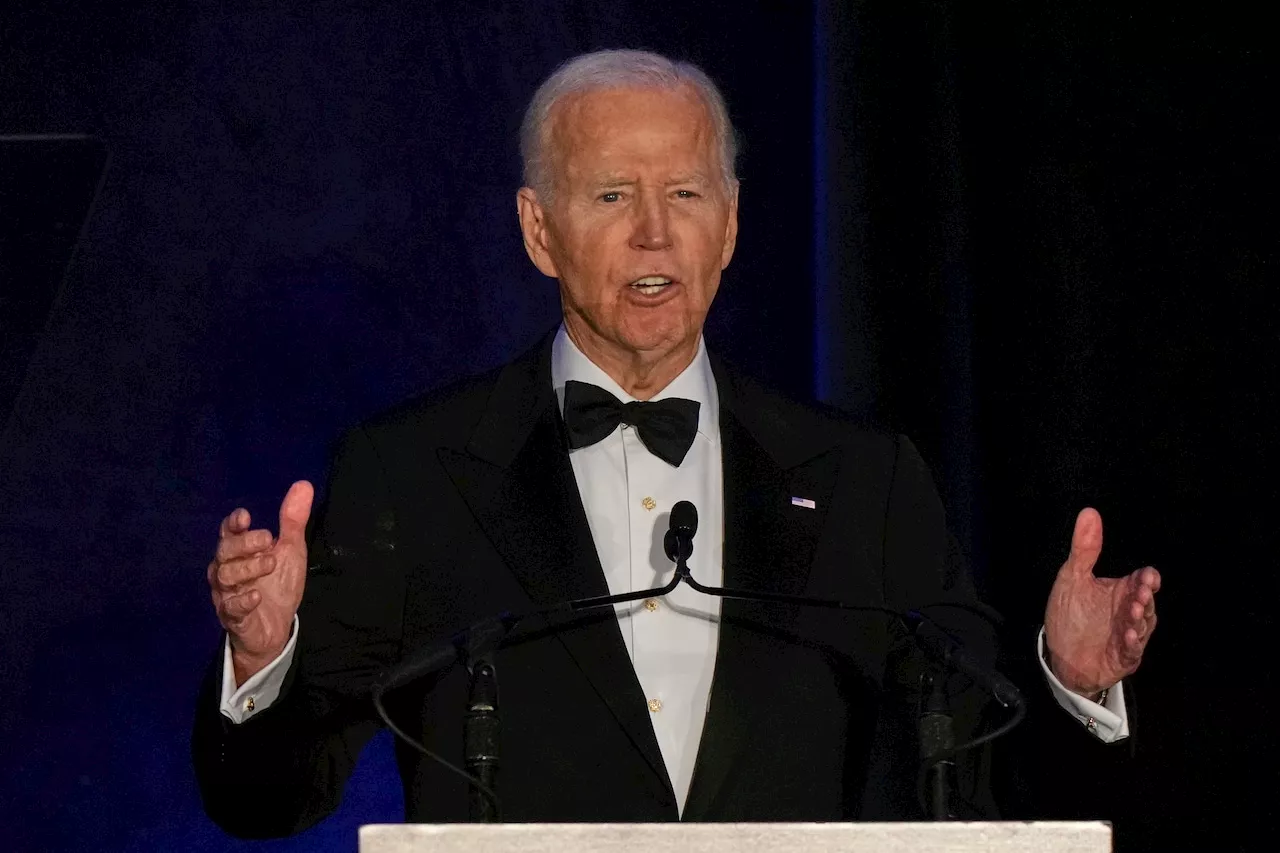
In a significant related event, Joe Biden, the former President of the United States, is currently undergoing radiation and hormone therapy for an aggressive form of prostate cancer. His office confirmed that the cancer, characterized by a high Gleason score and bone metastasis, was diagnosed in May 2025. This high-profile case highlights the importance of early detection and treatment options available for individuals facing this disease.