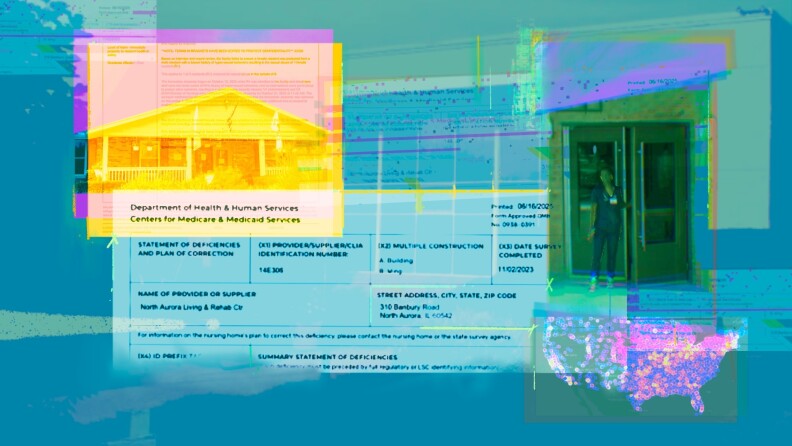
Concerns surrounding the placement of individuals with serious mental health issues in nursing homes have come to the forefront following a troubling incident at the North Aurora Care Center in Illinois. After being admitted in October 2023, a 28-year-old man identified only as V.R., who had diagnoses of schizophrenia and cognitive delays, allegedly assaulted multiple residents within 24 hours of arriving. The facility’s staff expressed reservations about his admission, stating, “We did not want to take this guy,” emphasizing that they felt ill-equipped to meet his needs.
Despite these concerns, officials from Petersen Health Care, the center’s corporate owner, overruled staff objections and proceeded with V.R.’s admission. In the early hours after his arrival, V.R. reportedly groped a resident with Down syndrome and attempted to enter the rooms of other female residents. Alarmingly, nurses on duty only became aware of these incidents through resident reports the following morning. V.R. was later found not guilty of battery due to his mental health condition, which has raised significant questions about the adequacy of care in facilities housing individuals with serious mental illnesses.
Systemic Issues in Mental Health Care
The situation at North Aurora is emblematic of a larger issue in the nursing home system, where facilities are increasingly accommodating individuals with various mental health disorders. According to an investigation by the APM Research Lab, approximately one in five nursing home residents in the United States — about 217,000 individuals — suffers from a serious mental illness, which includes conditions like schizophrenia and bipolar disorder. The study found that some nursing homes have upwards of 90% of residents diagnosed with such disorders.
Illinois law mandates that nursing homes establish a certification program to ensure they are equipped to care for residents with serious mental illnesses. However, the Illinois Department of Public Health has not certified any nursing home under this requirement since its enactment in 2010. This lack of oversight raises critical concerns about the safety and well-being of residents in facilities that may not have the necessary resources or training to address the needs of those with mental health challenges.
The journey of individuals like V.R. to nursing homes often begins with hospitalizations for physical or mental health crises. Many face barriers to accessing appropriate community-based care, leading to placements in nursing homes that may not be equipped to provide the specialized support they require. The absence of adequate home-based services and long waiting lists for mental health care exacerbate the problem, pushing vulnerable individuals into institutional settings where their needs may go unmet.
Impact of Staffing and Resources
Research indicates that nursing homes generally excel in providing physical care but struggle significantly with the mental health needs of residents. This disparity can lead to worsening conditions for individuals who may already be vulnerable. In some cases, the lack of appropriate care results in residents becoming a danger to themselves or others. For instance, a tragic incident in Kansas City in 2023 involved the death of a physically frail resident, allegedly attacked by another resident with serious mental illness.
The staffing levels at nursing homes also play a crucial role in the quality of care provided. In 2023, North Aurora was cited for having nurse staffing levels below federal minimum standards, which directly impacts the facility’s ability to manage residents with complex needs. A report indicated that Petersen Health Care faced significant financial challenges, which contributed to staffing shortages across its facilities.
Inadequate staffing often results in insufficient supervision and care, leading to increased instances of abuse and neglect. A Wisconsin case highlighted how a staff member exploited residents financially, dismissing concerns due to perceived paranoia related to their mental health conditions. Such incidents underline the urgent need for reform within the nursing home system, particularly as it pertains to residents with mental illnesses.
As the situation at North Aurora illustrates, the intersection of mental health and nursing home care is fraught with challenges. Advocates argue for a shift toward community-based care solutions rather than relying on institutions ill-suited for mental health treatment. U.S. Representative Daniel Goldman has proposed legislation aimed at facilitating Medicaid funding for home-based mental health care, reflecting a growing recognition of the need for systemic change.
As V.R. has been committed to a state-run treatment center for individuals with similar conditions, it emphasizes the necessity for targeted care that understands and addresses the complexities of mental health issues. The tragic events at North Aurora serve as a stark reminder of the ongoing challenges faced by both residents and facilities, and the urgent need for legislative and systemic reforms to ensure safety and adequate care in nursing homes.