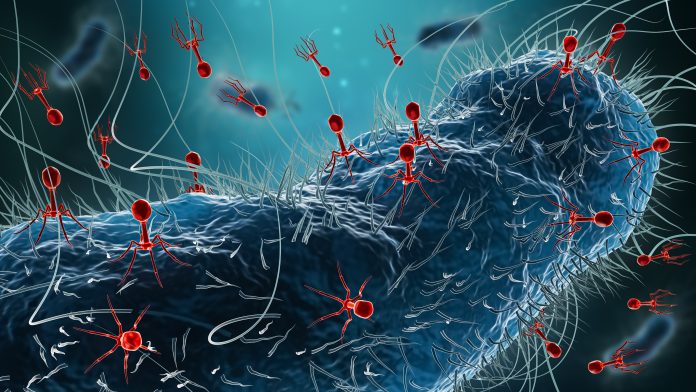
Researchers have made a significant breakthrough in understanding the human gut’s virome, uncovering hundreds of previously uncharacterized bacteriophages. This new study, published in the journal Nature, highlights the complex interactions between these viruses and gut bacteria, which could have important implications for gut health and various diseases.
Led by Professor Jeremy Barr from Monash University’s School of Biological Sciences, the study is the first to employ a large-scale, culture-based approach to isolate and examine temperate bacteriophages found in the human gut. The findings indicate that these phages may play a crucial role in the gut microbiome, significantly influencing conditions such as inflammatory bowel disease (IBD).
Understanding the dormant nature of gut bacteriophages is essential. The research team worked with 252 bacterial isolates sourced from the Australian Microbiome Culture Collection (AusMiCC). They cultivated these isolates in anaerobic chambers and subjected them to various conditions using ten different compounds. The study revealed that only 18% of computationally predicted prophages could be induced in pure cultures, indicating a previously hidden complexity.
A notable aspect of the study is the activation of these dormant phages. When exposed to human gut cells, the activation rate increased significantly. The researchers constructed a synthetic microbiome comprising 78 members, which, when co-cultured with human colonic cells (Caco2), activated 35% of phage species. This suggests that human biology plays a direct role in shaping the viral ecosystem of the gut.
The research identified that certain compounds, including Stevia—a common plant-based sugar substitute—and substances released by gut cells, are potent activators of gut phages. “We’ve known that the gut is full of viruses, but until now, we didn’t have the tools to study them in the lab,” said Sofia Dahlman, a graduate student in the Barr lab. “Our findings suggest that the human host isn’t just a passive environment; it actively influences viral behavior.”
Additionally, using CRISPR-based genetic engineering, the researchers identified mutations in viral genes that prevent activation. This insight into viral dormancy could inform future therapeutic strategies aimed at manipulating the gut microbiome for improved health outcomes.
“Being able to grow these viruses allows us to understand their function and provides the opportunity to develop microbiome therapeutics for diseases ranging from IBD to cancers,” noted Forster, a member of the research team. The technology also opens avenues for engineering probiotic strains with specific viral functions, potentially offering new pathways for treating gut-related diseases.
This study lays the groundwork for future research into the gut’s virome, marking a pivotal step in the quest to understand how these interactions affect human health. As we continue to uncover the complexities of our microbiome, the implications for treatment and understanding of gut health are profound.