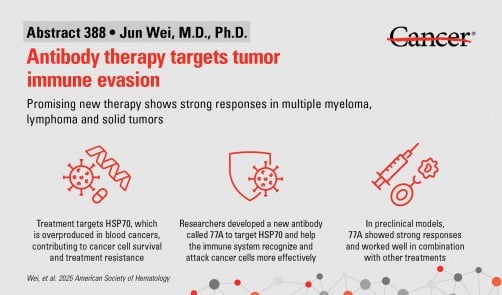
Researchers at The University of Texas MD Anderson Cancer Center have developed a promising new antibody therapy, known as **77A**, which has demonstrated the ability to enhance immune responses against various types of cancers. The therapy specifically targets a protein called **HSP70**, which is often produced in excess by tumors to evade the immune system. The findings were presented on **December 6, 2025**, at the **67th American Society of Hematology (ASH) Annual Meeting and Exposition**.
Leading the study, **Jun Wei**, M.D., Ph.D., an assistant professor in Lymphoma and Myeloma, and principal investigator **Robert Z. Orlowski**, M.D., Ph.D., a professor in the same department, highlighted the antibody’s potential to combat treatment resistance in blood cancers, such as myeloma and lymphoma, as well as solid tumors. Wei emphasized the significant implications of 77A, stating, “There is tremendous promise in the way 77A is capable of rewiring the immune system, enabling it to respond effectively against multiple cancers.”
Mechanism of Action
The **77A** antibody functions by targeting **HSP70**, a heat shock protein that plays a critical role in helping tumors maintain a favorable environment by suppressing immune responses. In laboratory models, this innovative therapy significantly enhanced the activity of both innate and adaptive immune cells, including **natural killer (NK) cells** and **T cells**. By improving the detection and destruction of cancer cells, 77A showed strong antitumor effects and worked effectively in conjunction with established treatments like chemotherapy, radiation therapy, and immune checkpoint blockade.
Moreover, early tests with human immune cells revealed that 77A could bolster immune responses in healthy donors, indicating its potential for broader application in clinical settings. The therapy also showed promise in combination with **adoptive T cell therapy**, a strategy where patients receive engineered immune cells designed to target cancer.
Future Directions
The success of 77A in various laboratory models sets the stage for its advancement into clinical trials. Orlowski stated, “These results give us confidence that 77A could become a versatile immunotherapy. Our next step is to advance a humanized version of this antibody into clinical trials to evaluate its potential in patients across multiple cancer types.”
The humanized version of the **77A** antibody is currently under development, with plans to initiate clinical trials in the near future. This research was supported by **Blood Cancer United** (formerly the Leukemia & Lymphoma Society), which underscores the growing collaboration between academic institutions and organizations focused on improving cancer treatments.
As the potential of 77A unfolds, it represents a significant step forward in the quest for effective cancer therapies, highlighting the importance of innovative approaches in reshaping treatment landscapes for patients battling these challenging diseases.